CHRONIC LYMPHOCYTIC
LEUKEMIA (CLL)
Exploring dysfunctional pathways, mechanisms, and biomarkers in CLL to
discover new insights into the progression of the disease.1
- Anderson MA, Huang D, Roberts A. Targeting BCL2 for the treatment of lymphoid malignancies. Semin Hematol. 2014;51(3):219-227.
- Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Allen C, Barber RM, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: A systematic analysis for the Global Burden of Disease Study. JAMA Oncol. 2017;3(4):524-548.
- Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2017, National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/csr/1975_2017/, based on November 2019 SEER data submission, posted to the SEER web site, April 2020.
- Stilgenbauer S, Furman RR, Zent CS. Management of chronic lymphocytic leukemia. Am Soc Clin Oncol Educ Book. 2015:164-175.
- Zhang S, Kipps TJ. The pathogenesis of chronic lymphocytic leukemia. Annu Rev Pathol. 2014;9:103-118.
- Guieze R, Wu CJ. Genomic and epigenomic heterogeneity in chronic lymphocytic leukemia. Blood. 2015;23:445-453.
- Hamblin TJ, et al. Unmutated Ig V(H) genes are associated with a more aggressive form of chronic lymphocytic leukemia. Blood. 1999;94(6):1848-1854.
- Hallek M, et al. iwCLL guidelines for diagnosis, indications for treatment, response assessment, and supportive management of CLL. Blood. 2018 Jun 21;131(25):2745-2760.
- Stilgenbauer S, Schnaiter A, Paschka P, et al. Gene mutations and treatment outcome in chronic lymphocytic leukemia: results from the CLL8 trial. Blood. 2014;123(21):3247-3254.
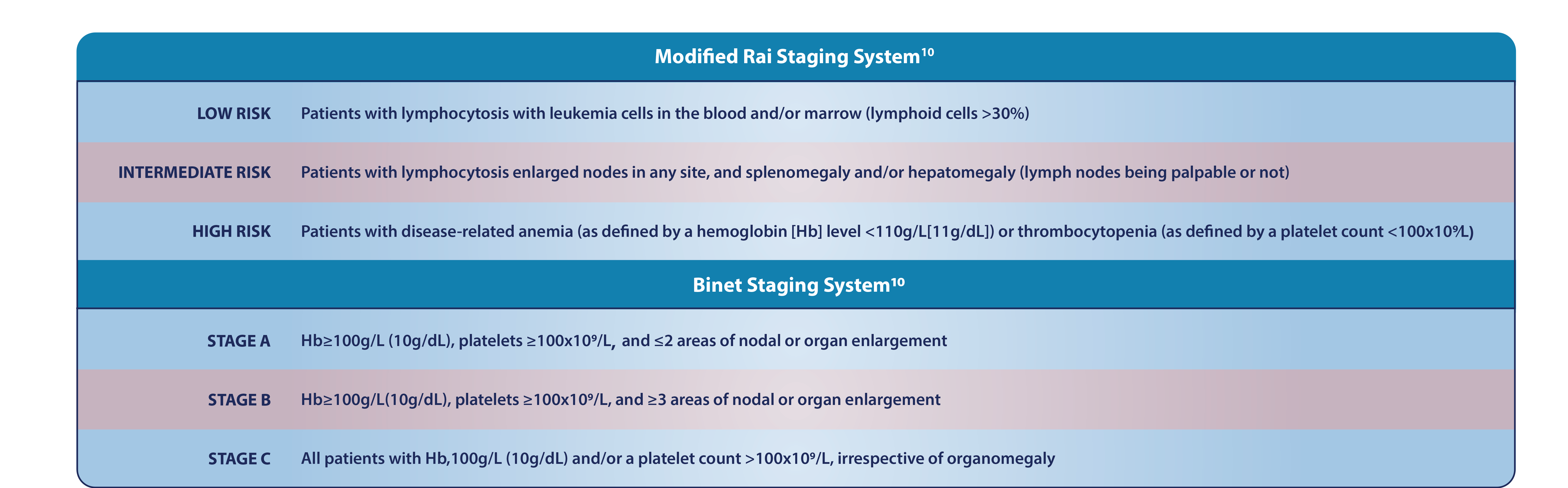
- Hallek M, Cheson BD, Catovsky D, et al. Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the International Workshop on Chronic Lymphocytic Leukemia updating the National Cancer Institute–Working Group 1996 guidelines. Blood. 2008;111(12):5446-5456.
- Bewarder M, et al. Current Treatment Options in CLL. Cancers (Basel). 2021;13(10):2468.
- Davids MS. How should we sequence and combine novel therapies in CLL? Hematology Am Soc Hematol Educ Program. 2017 Dec 8;2017(1):346-353.
- Bose P, Gandhi V. Recent therapeutic advances in chronic lymphocytic leukemia. F1000Res. 2017 Oct 31;6:1924.
- Lu K, Wang X. Therapeutic advancement of chronic lymphocytic leukemia. J Hematol Oncol. 2012;5(55).
- Hanada M, Delia D, Aiello A, Stadtmauer E, Reed JC. Bcl-2 gene hypomethylation and high-level expression in B-cell chronic lymphocytic leukemia. Blood. 1993;82(6):1820-1828.
- NCI. Cancer Stat Facts: Chronic Lymphocytic Leukemia (CLL). https://seer.cancer.gov/statfacts/html/clyl.html. Accessed March 2023.
- Scarfo L. Novel therapies and combinations in CLL refractory to BTK inhibitors and venetoclax. Hematology Am Soc Hematol Educ Program (2022) 2022 (1): 316–322.